For thousands of home care providers across the U.S., Medicaid funding isn’t just paperwork; it’s the difference between care happening or not. When a caregiver shows up to help an older adult with bathing, medications, or mobility, that visit is often made possible because Medicaid is quietly supporting it behind the scenes.
Now, a major federal law, known as the One Big Beautiful Bill Act (H.R. 1), is changing how that support works. You may have heard whispers about it in industry groups, caregiver chats, or agency meetings. You may have even felt the worry start to spread:
- What does this mean for home care?
- Will clients lose coverage?
- Will agencies be able to stay operational?
- How much more administrative work is coming?
The truth is, Home care relies heavily on Medicaid funds, and this bill significantly reshapes Medicaid rules over the coming years.
While some changes are gradual, the impact is real. Understanding it early gives agencies and caregivers a chance to prepare rather than react.
This blog is your clear, human-to-human explanation of what’s happening and what it means.
Quick Summary: What Is the One Big Beautiful Bill?
The One Big Beautiful Bill Act (H.R. 1) is a massive federal law passed in 2025. It covers everything from taxes to agriculture, but one of its biggest areas of impact is health care, especially Medicaid.
In simple terms, what the bill aims to do:
- Reduce federal spending on Medicaid and other government programs
- Introduce stricter eligibility rules
- Require more frequent Medicaid checks
- Shift more responsibility to states, agencies, and providers
- Adjust or tighten reimbursement models
Why it matters to home care
Since the home care industry relies heavily on Medicaid-funded Home and Community-Based Services (HCBS), even small changes to eligibility or reimbursement can have ripple effects.
Timeline (Important)
Most health-related changes do not start immediately.
- New Medicaid eligibility checks begin December 31, 2026
- Additional rules and adjustments will roll out through 2027-2028
This gives room to prepare, but not much room to delay.
At a Glance
Policy Type | Federal budget and healthcare reform law |
Impact Area | Medicaid eligibility, reimbursement, documentation, compliance |
Status | Enacted July 2025 |
Who It Affects | Medicaid recipients, home care agencies, caregivers, billing teams, compliance departments |
Why the Home Care Industry Is Paying Attention?
Home care is one of the most Medicaid-dependent healthcare sectors in the U.S. Unlike hospitals or private clinics, home care agencies don’t have a broad payer mix. Many rely on Medicaid for 60% to 90% of their revenue.
Combine this with:
- A rapidly growing aging population
- Increased demand for caregivers
- Higher operational costs
- Existing staffing shortages
- Tight reimbursement rates
It becomes clear why every new Medicaid rule matters.
Stat Callout
Over 4.5 million individuals rely on Medicaid-funded Home and Community-Based Services (HCBS), including seniors, people with disabilities, and medically fragile populations.
Any disruption to coverage or eligibility affects not only agencies but also families who depend on these services to keep loved ones safe at home.
Key Changes the Bill Introduces
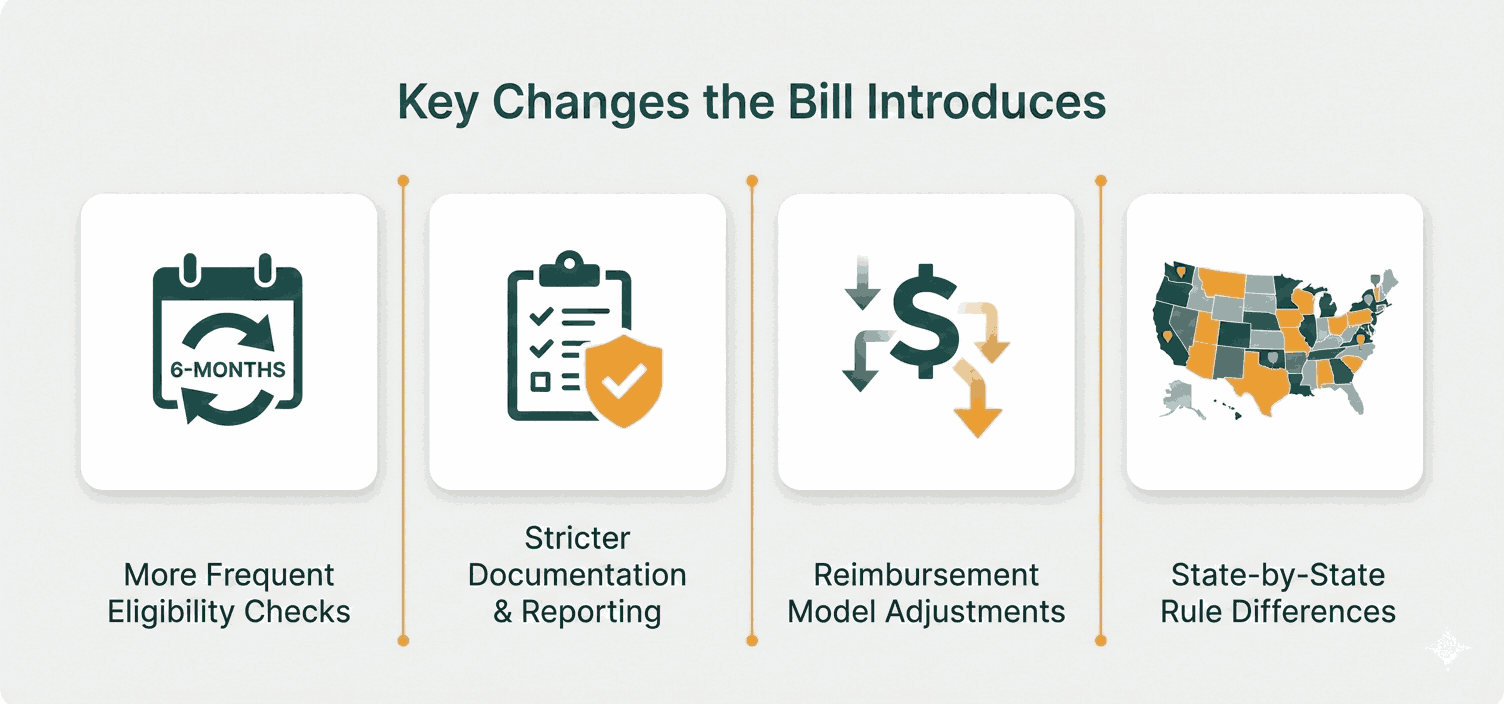
Here are the most relevant changes home care providers should understand:
Medicaid Eligibility Will Be Checked More Frequently
Under previous rules, many states reviewed eligibility annually.
Under the One Big Beautiful Bill:
- States must re-verify eligibility every 6 months
- Some states may choose to verify even more often
This means:
- More clients are losing coverage mid-service
- More administrative work
- More billing complications
Stricter Documentation & Reporting
Agencies must maintain:
- Real-time documentation
- Proof of service
- Accurate time logs
- Correct Medicaid identifiers
- Updated care plans
Compliance errors will be flagged faster, and denied claims will increase.
Adjustments to Reimbursement Models
Federal Medicaid funding levels are expected to decrease over the decade, affecting:
- HCBS funding pools
- Waiver program budgets
- State reimbursement rates
- Payment timelines
Greater State Interpretation & Flexibility
States will manage and apply rules differently. Two agencies in two different states may experience entirely different situations:
- Timelines
- Verification processes
- Reimbursement changes
- Audits
Who Will Be Most Affected?
Clients & Families
- More risk of losing Medicaid coverage
- More documentation needed
- Possible service interruptions
- Increased stress when coverage lapses
Empathy Moment:
Families already juggling care responsibilities don’t need more paperwork, but unfortunately, the burden is increasing.
Home Care Agencies
- Increased billing complexity
- Higher compliance standards
- More frequent eligibility checks
- Operational strain on small and mid-size agencies
Empathy Moment:
Most agency owners entered this field to help people, not to manage government paperwork, but compliance is becoming unavoidable.
Caregivers

- Possible changes in schedule stability
- Pay inconsistencies if claims are delayed
- More pressure to complete timely notes
Empathy Moment:
Caregivers already face low pay and burnout; administrative chaos only adds to the strain.
Short-Term vs. Long-Term Industry Impact
Short-Term (0–12 Months After Rollout)
Agencies can expect:
- Confusion as states interpret the bill
- Disruptions due to coverage lapses
- Increased time spent verifying eligibility
- Temporary delays in claims
- A need for staff retraining
Long-Term (1–5 Years)
The industry may shift toward:
- Hybrid funding models (Medicaid + private pay)
- More emphasis on accountability
- Better documentation systems
- Increased adoption of digital platforms
- Higher compliance standards
The home care industry will adapt as demand for care continues to grow.
Challenges And Opportunities
Challenges
- Higher administrative cost
- More front-office staffing pressure
- Increased documentation burden
- More compliance tracking
- More denied claims
Opportunities
- Encouraging modernization
- Digitizing workflows
- Reducing errors through automation
- Improving quality through standardized care plans
- Using data to strengthen reimbursement processes
Change can be disruptive, but it can also accelerate innovation.
The Role of Technology in Adapting to the New Bill
With stricter Medicaid rules, agencies cannot afford manual processes anymore.
Technology plays a huge role in:
- Automating documentation
- Ensuring time logs and session notes meet state rules
- Keeping care plans updated
- Running real-time eligibility checks
- Preventing claim denials
- Tracking compliance for audits
Industry Trend:
Manual documentation is dying, and automation is becoming the new standard. Agencies that digitize early will experience fewer disruptions as HR1 rolls out.
Stop Manual Work. Prevent Denials. Simplify Operations with Caretap
How Providers Can Prepare Now?
Here’s HR1 Readiness Checklist:
- Evaluate your payer mix, identify Medicaid dependency
- Train billing and admin teams on new documentation rules
- Standardize caregiver notes and time logs
- Monitor state-specific HR1 implementation updates
- Adopt Medicaid-friendly care management software
- Implement internal audit processes
- Prepare families for possible mid-year eligibility checks
- Strengthen communication between scheduling, billing, and caregiving teams
Conclusion: The Future of Home Care Isn’t Slowing Down
The One Big Beautiful Bill is large, complex, and full of changes, but it is not the end of home care. The industry has survived shifting policies for decades, and it will continue to evolve.
Two truths stand out:
- Change is coming, but you have time to prepare.
- Organizations that modernize, automate, and stay compliant will be the ones that adapt fastest.
- Home care is essential.
- Families need it.
- Caregivers are the backbone of it.
- Policy shifts may shape how agencies operate, but they won’t erase the need for care.
The future of home care remains strong, and with the right preparation, agencies will not just survive this change but emerge stronger, more efficient, and more resilient.



